When we think of pre-surgical ablutions, and general antiseptic procedures, we generally think of the British Quaker Joseph Lister (for whom Listerine is named), but the man who first realized that it might be a good idea for doctors to scrub up was a Catholic obstetrician who was ostracized from the medical profession and died impoverished in a mental asylum.
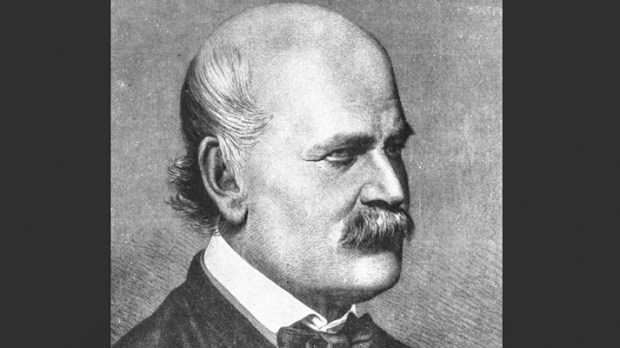
Ignaz Philipp Semmelweis (1818-1865) was the fifth of 10 children born to a wealthy German grocer living in Hungary. At the age of 19, he commenced studies in law at the University of Vienna, but switched to medicine, completing his doctorate in 1844. Semmelweis applied to a clinic for internal medicine but failed to secure a position, so he decided to specialize in obstetrics.
In 1846, Semmelweis started working in the First Obstetrical Clinic of the Vienna General Hospital, which had two maternity clinics. These provided free services to women bearing illegitimate children, in hopes of reducing rates of infanticide.
The First Clinic had an average maternal mortality rate of about 10% due to puerperal fever (fever caused by uterine infection following childbirth). The Second Clinic’s rate was considerably lower, averaging less than 4%. This fact was known outside the hospital. The two clinics admitted on alternate days, but women begged to be admitted to the Second Clinic, due to the bad reputation of the First Clinic. Semmelweis described desperate women begging on their knees not to be admitted to the First Clinic. Some women even preferred to give birth in the streets, pretending to have given sudden birth en route to the hospital (a practice known as street births), which meant they would still qualify for the child care benefits without having been admitted to the clinic. Semmelweis was puzzled that puerperal fever [a leading cause of death in childbirth] was rare among women giving street births. “To me, it appeared logical that patients who experienced street births would become ill at least as frequently as those who delivered in the clinic. […] What protected those who delivered outside the clinic from these destructive unknown endemic influences?” Semmelweis was severely troubled that his First Clinic had a much higher mortality rate due to puerperal fever than the Second Clinic. It “made me so miserable that life seemed worthless.” The two clinics used almost the same techniques, and Semmelweis started a meticulous process of eliminating all possible differences, including even religious practices. The only major difference was the individuals who worked there. The First Clinic was the teaching service for medical students, while the Second Clinic had been selected in 1841 for the instruction of midwives only. (Ignaz Semmelweis, Etiology, Concept and Prophylaxis of Childbed Fever [1861])
Finally, a personal tragedy led to Semmelweis’ groundbreaking discovery. Semmelweis left for Venice in March 1847 to take a break from work. Upon his return:
I was immediately overwhelmed by the sad news that Professor [Jakob] Kolletschka, whom I greatly admired, had died in the interim.The case history went as follows: Kolletschka, Professor of Forensic Medicine, often conducted autopsies for legal purposes in the company of students. During one such exercise, his finger was pricked by a student with the same knife that was being used in the autopsy … Kolletschka contracted lymphangitis and phlebitis [inflammation of the lymphatic vessels and of the veins respectively] in the upper extremity. Then […] he died of bilateral pleurisy, pericarditis, peritonitis, and meningitis [inflammation of the membranes of the lungs and thoracic cavity, of the fibroserous sac surrounding the heart, of the membranes of the abdomen and pelvic cavity, and of the membranes surrounding the brain, respectively]. … I could see clearly that the disease from which Kolletschka died was identical to that from which so many maternity patients had also died. The maternity patients also had lymphangitis, peritonitis, pericarditis, pleurisy, and meningitis… (Ignaz Semmelweis, Etiology, Concept and Prophylaxis of Childbed Fever [1861], translated by K. Codell Carter [1983])
Semmelweis postulated that puerperal fever was a form of blood poisoning or pyaemia caused by “cadaverous particles” on the hands of examining physicians who had conducted autopsies or pathological dissections without having a thorough wash afterward. He introduced a policy of washing hands with a solution of chlorinated lime (calcium hypochlorite). The maternal mortality rate dropped from 18.3 percent in April 1847 to zero the following year.
Despite the evidence in favor of Semmelweis’ theory, it was roundly rejected by scholars and doctors across Europe, who clung stubbornly to ancient Greek and Roman medical concepts like “the four humors,” and treated childbed fever with bloodletting and purging. Semmelweis disliked public speaking and writing, so it was difficult to secure recognition of his discovery. Furthermore, following the 1848 Hungarian Revolution, Hungarians were mistrusted in Austria. Semmelweis lost his job and, infuriated, started writing open letters to prominent obstetricians, accusing them of being irresponsible murderers. They and his wife thought that he was going mad, and in 1865, Semmelweis was consigned to an asylum, where he died, ironically, of pyaemia after severe beatings from the guards.
Germ theory only became widely accepted following the experiments of the devout French Catholic Louis Pasteur, founder of physio-chemistry, father of bacteriology and inventor of pasteurization. The British Quaker Lister acted on Pasteur’s research and carbolic acid (phenol) became the first widely-used antiseptic in surgery.
Today, as you wash up, spare a prayer for the physicians who saved lives by this simple act, especially Ignaz Semmelweis.